Paige’s hidden Brain AVM claimed her life when she was just 6 years old.
Dr's told us Paige’s AVM was present at birth. With early detection, treatment was possible - her life could have been saved.
Signed in as:
filler@godaddy.com
Dr's told us Paige’s AVM was present at birth. With early detection, treatment was possible - her life could have been saved.
In 2018, our lives changed forever when we lost our beautiful 6-year-old daughter, Paige, to an undetected brain arteriovenous malformation (AVM).
That morning, Paige went off to school happy, healthy, and full of life. A few short hours later, I got a call from the school nurse: Paige had a severe headache. Minutes later, before I even reached the end of our block, another call came — Paige was unresponsive, and 911 had been called.
I never heard my daughter’s voice again. Within hours, Paige was gone.
Doctors explained she had been born with this condition. Then came the words that haunt me still:
“If you had known Paige had an AVM, it could have been treated. Paige would likely still be here today.”
Those words are why I founded The Paige Elizabeth Keely Foundation.
Brain AVMs are often treatable if detected early. Yet, most AVMs and aneurysms show little to no symptoms until it’s too late. That is why early detection and awareness are critical — so no other family has to endure the loss we carry every day.


Together, The Paige Elizabeth Keely Foundation and Stony Brook Hospital’s Mofakham-Mikell Laboratory in the Neurology Department, have launched a groundbreaking collaboration: funding a dedicated Fellowship Program focused exclusively on the study focused on the early detection of brain AVMs, aneurysms, and other life-threatening neurological conditions.
This level of research has never existed before. The knowledge gained will change the future of detection, treatment, and prevention — impacting countless lives.
Our AVM research project is moving forward rapidly, powered by the dedication of our exceptional research team and the esteemed physicians of Stony Brook Hospital’s Mofakham-Mikell Laboratory in the Neurology Department.
Your generous donation will help raise awareness, fund groundbreaking research, and honor lives impacted by these silent conditions.

Dr. Sima Mofakham

Dr. Chrles Mikell

Dr. Morsal Mosallami Aghili



Developing Non-Invasive Imaging Methods to Detect Brain AVM Before Rupture.
Our groundbreaking AVM Research strives to identify AVMs before rupture through innovative imaging methods. We are also advancing 3D modeling, rupture risk analysis, and other critical projects — all aimed at improving care and saving lives.


AVM's are abnormal tangle of blood vessels in a child’s brain where arteries connect directly to veins, bypassing the normal capillary system. This disrupts normal blood flow and increases the risk of bleeding in the brain (hemorrhage).
AVMs in children are rare but serious, as they can grow and change over time. They are often silent, showing no symptoms until problems occur — such as seizures, headaches, or, in severe cases, rupture.
With early detection and treatment, many pediatric AVMs can be managed or corrected, helping prevent life-threatening complications.


If a doctor suspects an AVM, they will perform a complete medical exam and may order imaging tests to confirm the diagnosis.
Common tests include:

Most researchers believe that Brain AVMs are congenital, meaning they are usually present at birth. They are thought to form in utero during early brain and blood vessel development, when arteries and veins are supposed to connect through tiny capillaries but instead form a tangled, abnormal connection.
However, the exact cause is still uncertain. While most AVMs are believed to arise before birth, some experts suggest they may also develop or change after birth.

Hereditary Hemorrhagic Telangiectasia (HHT) is a rare genetic disorder that affects blood vessels. People with HHT develop abnormal connections between arteries and veins, called telangiectasias and arteriovenous malformations (AVMs), which can occur in various organs — including the brain, lungs, and liver.
For individuals with HHT, the risk of developing a brain AVM is dramatically higher — estimated to be up to 10,000 times greater than in the general population. Because of this strong correlation, children and adults with HHT are often screened with imaging tests to detect AVMs early, even before symptoms appear.
Why this matters:
Hereditary Hemorrhagic Telangiectasia (HHT) is diagnosed through a combination of clinical evaluation, family history, and genetic testing!
SIGNS & SYMPTOMS
A diagnosis is considered:
Genetic testing can confirm HHT by identifying mutations in specific genes (most commonly ENG, ACVRL1, or SMAD4).
Because of this inheritance pattern, screening family members is critical once HHT is diagnosed, especially to check for AVMs in the brain, lungs, or liver.

The Paige Elizabeth Keely Foundation is a nonprofit 501c3 (EIN-84-5024812) organization created in Paige’s honor.
Our goals:

On April 29, 2019, Tyler went to school and was picked up by his dad, just like any ordinary day. Later, he asked to be dropped off at the neighborhood park to play basketball with friends. His mom left him there, saying, “I’ll see you in a little while.”
Less than five minutes later, Tyler texted her asking to come back because he had a bad headache. By the time she returned just three minutes later, Tyler was already losing function in his arms and legs, and his pupils were severely dilated.
At the ER, doctors found bleeding in Tyler’s brain. The bleeding worsened over the next few hours and eventually clotted. Tyler had suffered from a ruptured Arteriovenous Malformation (AVM). Despite every effort, he was declared brain dead. His family was told there was nothing more that could be done.
As Tyler’s family sat in the hospital praying for a miracle, they were introduced to the organ donation nonprofit LiveOnNY. His mother knew in her heart that Tyler would want to save lives if he had the chance — and he did. Tyler became a hero, saving the lives of many through organ donation.
August 20, 2019, Danielle started what seemed like a typical summer day. She went to camp full of excitement, dressed and ready to take part in color war. Just two hours later, she told her counselors she was having trouble moving her right leg and asked to be carried to the nurse’s office. That’s when a horrific headache began.
The camp nurse quickly called 911, and Danielle was rushed to the hospital. A head CT revealed a large amount of blood in her brain, later determined to be from a ruptured AVM. She was flown to the local children’s hospital for further treatment, where she spent more than two weeks in the ICU.
Life changed instantly. Danielle couldn’t move her right leg and only began to regain slight movement in her right hand days after her first surgery. After recovering from two brain surgeries, she spent the next four weeks in intensive physical therapy, working to regain use of her right arm and leg.
Over the past year, Danielle has continued to fight through incredible challenges. In September 2020, approximately one year after her initial diagnosis, doctors discovered her AVM had grown back. She required another surgery to remove it completely.
Today, Danielle is working tirelessly in physical therapy to achieve every goal she has set for herself. An athletic and determined girl before her AVM rupture, she looks forward to returning to her passions — dance and gymnastics — and picking up right where she left off.

I’ve had three very severe and debilitating headaches (9.5 on the doctor’s 1-to-10 pain scale).
On Friday afternoon, I was supposed to fly to Montana for two weeks — the first to teach at IU Field Camp, the second for vacation at the cabin. While I was at the airport, waiting to board, my doctor called. Between tears I told her where I was. She told me not to get on the plane, to head immediately to the ER at Methodist, and to see a neurosurgeon. Not exactly calming words — but necessary.
I turned around, left the airport, and caught an Uber to the Med Center. Scott met me there. I spent the night in the ER while my luggage flew to Helena and back without me.
It was surreal. They ran two CT scans, both negative, which told the doctors that the blood seen on the MRI was old blood (not active bleeding). The MRI only showed blood but couldn’t explain the cause.
The doctors gave me two possible explanations:
Theory A: Some of my arteries may connect directly to veins without capillaries in between. Without the normal high-to-low pressure buffer, a blood vessel can burst. This can be tested with an angiogram, which they plan to do Tuesday.
Theory B: A tumor could be causing swelling and bleeding but is currently hidden or masked by the blood. To test this, I’ll need to wait until the blood reabsorbs into my body, then undergo another MRI in a month or two.

On Super Bowl Sunday (February 2, 2020), Jenna suddenly lost consciousness and stopped breathing. Her dad, Ryan, immediately administered CPR. At the local hospital, doctors realized the gravity of her condition and quickly medevaced her — with her mom, Kelly, by her side — to the regional pediatric ICU.
There, medical staff discovered an Arteriovenous Malformation (AVM) that had ruptured, causing major hemorrhaging in her brain. Two surgical interventions so far have kept her in the fight. Jenna was likely born with this condition, which had sat dormant until that day.
Just the day before, Jenna had played in her soccer game, spent time with friends and family, and showed no symptoms of distress.
Jenna’s AVM was located on the left side of her brain — the side that controls speech and mobility. Her mother, Kelly, never left her side and watched her daughter fight for her life for over 50 days.
Kelly shared: “It’s minute by minute, two steps forward, two steps back. Always keeping in the back of my mind the thought of planning my daughter’s funeral.”
Jenna is truly a miracle. The Sheehy family almost lost her twice, and no one on her hospital floor could believe what she has overcome.
On March 13, 2020, Jenna faced another terrifying hurdle — surgery to remove the AVM. After an extremely long and fragile procedure, her mother shared this message:
“Jenna is back in her room on the ICU floor and sleeping well. Thank God the AVM is successfully out of her head. She is a miracle, and I will continue to thank God for her every day.”
On March 28, 2020, after eight long weeks on an emotional rollercoaster no family should ever endure, Jenna was finally discharged. She left the hospital and began rehab, with a long road of recovery ahead.

When my daughter was born, we were told the mark on her ear was simply a birthmark. When she was almost two, it began to scab over, so I took her to the doctor. They said it was a hemangioma and referred us to a specialist.
The day we were scheduled to see that specialist, I was changing her clothes when her shirt tugged on her ear and pulled the scab off — she began to hemorrhage. We rushed to the doctor, where she was stabilized, kept overnight, and then sent home. Once again, we were told it was a hemangioma.
Just a week later, after waking from her nap, her scab had stuck to her pillow. When it pulled off, the bleeding started again. This time we called 911. The paramedics could not control the bleeding, and at the hospital a specialist had to place a stitch to stop it. Once she was stable, she was transferred to a larger hospital in the city, where she received a blood transfusion.
Doctors initially prepared to do a biopsy, but during the procedure they discovered the truth — she did not have a hemangioma. She had an Arteriovenous Malformation (AVM).
In early adolescence, I developed what appeared to be a birthmark under my left eye. My mother took me to my pediatrician, who assured her it was purely superficial and nothing to worry about. Throughout my childhood, I also developed “strawberry mark” hemangiomas, which doctors again said were not a concern.
Just a few months before turning 18, I had a Mirena IUD (a form of hormonal birth control) placed. I want to be clear — I do not blame the IUD for my AVM or the health issues that followed. I believe my AVM would have become symptomatic at some point regardless.
After the IUD was placed, the area around my left eye began to swell. I noticed pulsating, pain, and a bruit (a whooshing sound in my head). I waited longer than I should have to get checked, but in October 2010, two months after my 20th birthday, I finally received my diagnosis: an Arteriovenous Malformation (AVM).
Over the years, I underwent eight embolizations, a debridement for necrosis, a skin graft, a craniotomy, and gamma knife radiation. At the time of surgery, my AVM spanned from within my sinus and face to the inside of my skull and dura. The procedure to remove it was extensive, and although most of it was excised, about 2% remains in my sinus. My surgeon explained that removing it completely would have required a “catastrophic deconstruction” of my face.
Today, I am managing relatively well. My pain is under control, and I continue to see a therapist to help me cope with the lasting effects of my AVM journey, along with other challenges.
In early adolescence, I developed what looked like a birthmark under my left eye. My mother took me to my pediatrician, who assured her it was only superficial and nothing to worry about. Throughout childhood, I also developed “strawberry mark” hemangiomas, which doctors again dismissed as harmless.
Just a few months shy of turning 18, I had a Mirena IUD (hormonal birth control) placed. To be clear, I don’t blame the IUD for my AVM — I believe it would have become symptomatic at some point in my life regardless.
After the IUD was placed, the area around my left eye began to swell. I started experiencing pulsating, pain, and a bruit (the whooshing sound in my head). I waited longer than I should have to get checked, but in October 2010, two months after my 20th birthday, I was diagnosed with an Arteriovenous Malformation (AVM).
Altogether, I underwent eight embolizations, a debridement for necrosis, a skin graft, a craniotomy, and gamma knife radiation. At the time of excision, my AVM spanned from my sinus and face into my skull and dura. The surgery was extensive, and while most of the AVM was removed, about 2% remains in my sinus. My surgeon explained that removing it entirely would have required a “catastrophic deconstruction” of my face.
After surgery, I worked hard to rebuild my life. I returned to school, rejoined my Honors English class three years later, graduated high school, and later earned an Associate’s Degree. For many years, I lived a relatively normal life.
But on January 15 of this year, I had my first grand mal seizure. On January 27, I required a second brain surgery because doctors found an “offshoot” of my original AVM. Since I was so young when I had my first AVM removal in 2003, my brain was still developing, and part of it had been missed — it developed as my brain matured.
Now, I live with short-term memory loss and am prone to seizures, so I take multiple seizure medications. I sometimes struggle with comprehension and following spoken directions, though my speech sounds normal to others. Thankfully, my motor skills remain intact.
I’m still in recovery. My neurosurgeon told me it may take up to a year to heal, since this was my second brain surgery in the same area — and because of my age.
Please consider sharing your story. By doing so, you will help survivors understand that they are not alone in their struggles. Discussing your experiences can provide hope to others battling the aftermath of AVM ruptures.
You are a WARRIOR!
You emerged from this challenge, and that is a testament to your strength. While we cannot alter the past, we can take proactive steps together to raise awareness and combat BRAIN AVMs. Let us unite in this effort.
Please consider making a donation to the Paige Elizabeth Keely Foundation. We are a non-profit organization created in honor of our daughter Paige Keely. (501(c)(3)) (EIN: 84-5024812)
No family should have to go through the pain of losing a child when early detection could have kept our beautiful 6 year old here with us.
Through early detection and research other families can be spared the horrors that we endured.
Your generous gift allows us to pursue our mission:
-Raise awareness of Arteriovenous Malformation of the brain, (AVM)
-Fight for earlier detection
All contributions are tax deductible under applicable laws.

The Paige Elizabeth Keely Foundation
Saint James, New York 11780, United States
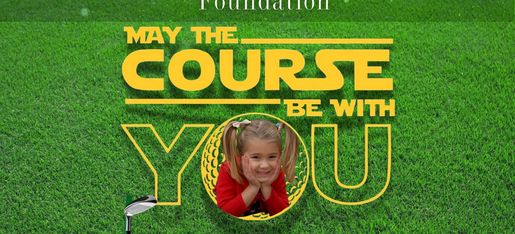
The 3rd Annual Paige Keely Golf Outing
“May the 4th Be With You”
📅 Monday, May 4th, 2026
📍 Nissequogue Country Club
This year, we’re honored to recognize
Gregory Tellone — Nissequogue Fire Chief & Owner of Continuity Centers.
A leader, protector, and community champion who embodies service in every way.
Grab your lightsabers (or, realistically… your golf clubs) and join us for an unforgettable day supporting lifesaving early detection research for AVMs & aneurysms through the Paige Elizabeth Keely Foundation.
Click the link for sponsorships & registration!
🎀✨🎀